Causes, Symptoms, and Surgery Options for Cataracts
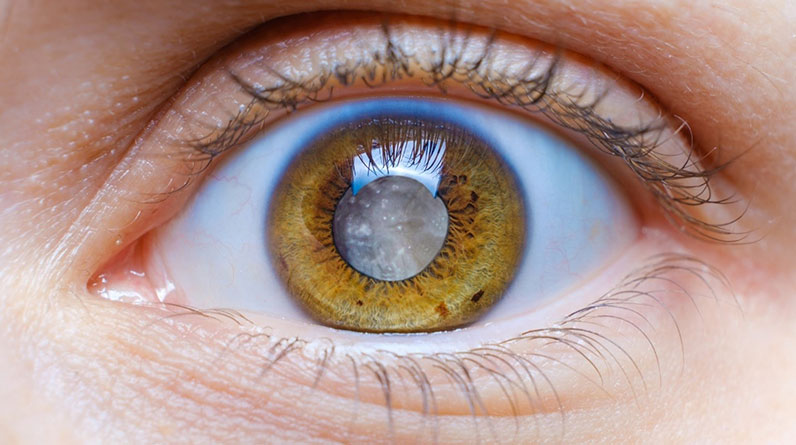
Cataracts are a common eye condition in which the normally clear lens of the eye becomes cloudy, leading to blurred vision and difficulty seeing clearly. This condition typically develops with age but can also result from injury, certain medications, or underlying health conditions.
Left untreated, cataracts can cause significant vision impairment, but the good news is that cataract surgery offers an effective solution for restoring vision.
In this article, we’ll explore the causes, symptoms, and treatment options for cataracts.
Causes of Cataracts
Cataracts develop when proteins in the lens of the eye break down and clump together, creating cloudy areas that impair vision. Several factors can contribute to this process, including:
1. Age-Related Factors
The most common cause of cataracts is aging. As we age, the natural proteins in the eye’s lens degrade and accumulate, causing the lens to become less transparent. Most people over 60 experience some degree of lens clouding, though it may not always impair vision immediately.
2. Genetic Predisposition
Family history can play a role in the development of cataracts. Individuals with close relatives who have had cataracts may be at higher risk, suggesting a genetic component to the condition.
3. Medical Conditions
Certain medical conditions increase the risk of cataracts, especially diabetes, which is a leading risk factor. In people with diabetes, elevated blood sugar levels can cause changes in the eye’s lens, speeding up cataract formation. Additionally, long-term use of corticosteroid medications and conditions like hypertension can also contribute to cataract development.
4. Environmental Factors
Prolonged exposure to ultraviolet (UV) radiation from the sun is another contributing factor. Over time, UV rays can damage the proteins in the eye’s lens, leading to cataract formation. Smoking and excessive alcohol consumption also accelerate the breakdown of lens proteins, further increasing the risk of cataracts.
5. Eye Injuries
Injuries to the eye, such as blunt trauma, chemical burns, or exposure to radiation, can cause cataracts to develop. These traumatic cataracts can form immediately after the injury or appear years later, depending on the extent of the damage.
Understanding these causes is essential for identifying risk factors and taking preventative steps to delay or manage the onset of cataracts.
Cataracts Surgery Options
When cataracts significantly impair vision and affect daily activities such as reading, driving, or recognizing faces, surgery becomes necessary. Cataract surgery is a highly effective and routine procedure that removes the cloudy lens and replaces it with a clear artificial lens (intraocular lens, or IOL). Here are the primary types of cataract surgery, along with the associated risk factors:
Types of Cataract Surgery
1. Phacoemulsification Phacoemulsification is the most common and advanced type of cataract surgery. During this procedure, a small incision is made in the cornea, and an ultrasound probe is inserted to break up the cataract into small pieces, which are then suctioned out. An artificial lens is inserted to replace the cloudy lens. Phacoemulsification is minimally invasive, allowing for a quicker recovery and less postoperative discomfort.
2. Extracapsular Cataract Extraction (ECCE) ECCE is typically used for advanced cataracts that are too dense for phacoemulsification. In this procedure, a larger incision is made to remove the cloudy lens in one piece. The artificial lens is then implanted in the same way as with phacoemulsification. While effective, ECCE requires a longer recovery time due to the larger incision.
3. Laser-Assisted Cataract Surgery In laser-assisted cataract surgery, a laser is used to make precise incisions in the cornea and break up the cataract before removing it. This method offers greater precision, which can lead to faster healing and a reduced risk of complications.
Risks Associated with Cataract Surgery
While cataract surgery is generally safe and successful, there are some risks, as with any surgical procedure:
- Infection: Though rare, infection can occur after surgery if bacteria enter the eye during or after the procedure. Antibiotic eye drops are typically prescribed to prevent this complication.
- Inflammation: Mild inflammation is common after surgery, is usually temporary, and can be treated with anti-inflammatory eye drops. Severe inflammation, though rare, may lead to complications if not managed properly.
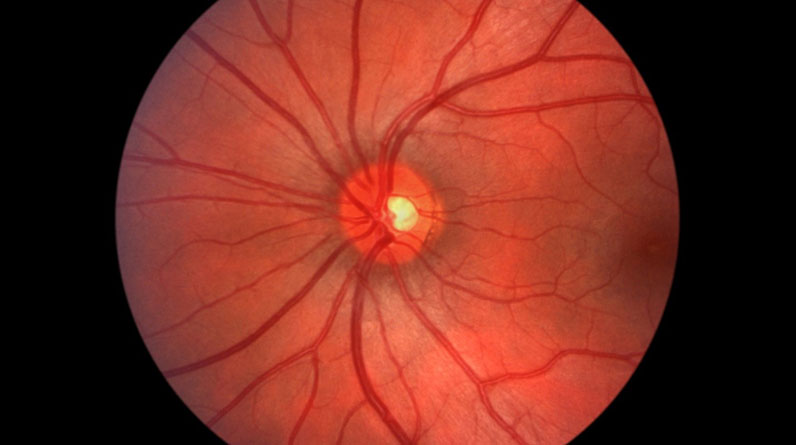
- Retinal Detachment: A more serious but uncommon complication, retinal detachment, can occur when the retina pulls away from its normal position after surgery. Symptoms include sudden flashes of light or a shadow in the visual field, requiring immediate medical attention.
- Secondary Cataracts (Posterior Capsule Opacification): In some cases, months or years after surgery, a condition called posterior capsule opacification (PCO) can develop. This happens when the membrane behind the new lens becomes cloudy, mimicking cataract symptoms. Fortunately, PCO can be treated quickly and painlessly with a laser procedure known as YAG laser capsulotomy.
Cataract surgery is a highly effective solution for restoring vision when cataracts become disruptive. For most people, cataract surgery significantly improves quality of life, leading to restored vision.
Early detection and timely treatment of cataracts are necessary for maintaining good vision and preventing the condition from severely impairing daily life. Regular eye exams help identify cataracts in their early stages, allowing for proactive management and reducing the risk of vision loss.
Cataract surgery, when necessary, is highly effective in restoring clear vision and improving quality of life. By recognizing symptoms early and exploring treatment options with an eye care professional, individuals can protect their vision and continue to enjoy a healthy, active lifestyle.